The Basics
How is an abdominal aortic aneurysm diagnosed?
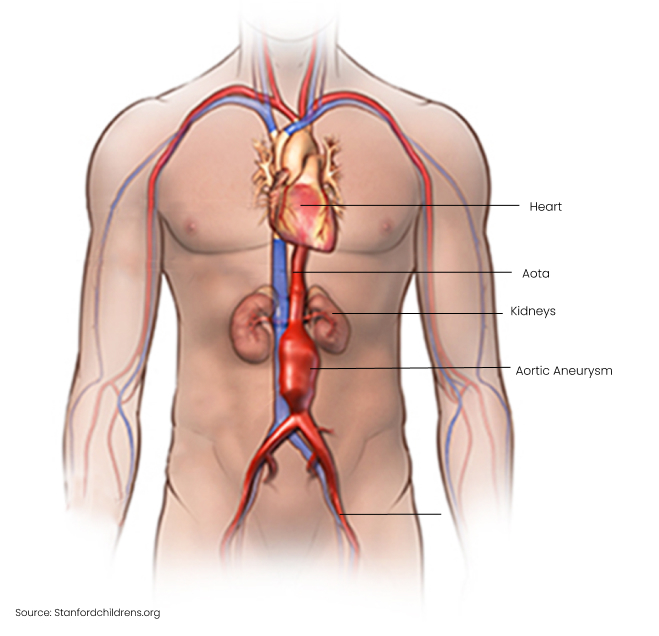
A routine physical examination of the abdomen may detect a large abdominal aortic aneurysm, but > 50% are not detected on examination because of the deep location of the aorta.
The easiest and most cost-effective test to diagnose an aortic aneurysm is an ultrasound scan. A CT scan is usually required when planning to fix an aneurysm, as it gives precise information that allows your surgeon to decide which method is most appropriate.
Screening for an abdominal aortic aneurysm
Most patients are unaware that they have an abdominal aortic aneurysm, as most aneurysms do not cause symptoms until it causes serious trouble like bursting (which most patients do not survive). It is, therefore, recommended that those at elevated risk get screened.
International recommendations are that the following groups get a once-off ultrasound screen:
- men between the ages of 65 and 75 years who smoked at any time in their lives
- men between the ages of 65 and 75 who never smoked but who have other risks, such as a family history of aneurysm or a personal history of heart attack, stroke, or peripheral artery disease
- women older than 65 years who have had a first-degree relative (sibling or parent) diagnosed with an aneurysm
What are the symptoms and signs of an aortic aneurysm?
The alarming thing about aortic aneurysms is that most do not cause any symptoms, and many burst with no warning. When there are symptoms, they are usually:
- Persistent pain in the back (or the sides of the lower back region), belly, or chest. Note: Sudden severe pain in these regions may mean that the aneurysm is about to rupture, especially if you feel faint and sweaty with a fast heartbeat. This is a medical emergency. Do not delay in getting emergency care.
- Noticeable swelling between the ribcage and belly button that pulses in rhythm with your heartbeat.
What increases the risk of an aortic aneurysm?
No single, specific cause has been identified that results in the weakening of the wall of the aorta, but there are several well-known risk factors:
- tobacco smoking – this is the strongest risk factor for aortic aneurysms
- high blood pressure
- age – the risk increases with advancing age, especially in those 65 years and older
- male gender – men are up to six times more likely to have an aneurysm than women
- atherosclerosis (the build-up of fatty plaques within the artery walls) and high cholesterol levels
- family history – if your siblings or parent has or had an aneurysm
- being overweight
- genetic factors or diseases which cause weakness in the walls of arteries.
How are aortic aneurysms managed?
All patients require best medical therapy, which involves treating the risk factors contributing to the development of an aneurysm or increasing the risk of rupture.
This involves both medication to treat conditions like diabetes, hypertension, and high cholesterol and healthy lifestyle changes that includes:
- Stop smoking.
- A healthy eating plan and regular exercise will help to manage other conditions like high blood pressure, high cholesterol, and diabetes, which increase your aneurysm risk.
- Maintenance of a healthy weight.
Assessment for surgery
Repair of the aneurysm is considered when the risk of rupture is higher than the risk posed by the surgical procedure. The bigger the aneurysm, the greater the risk of rupture.
Surgery should be considered if the aneurysm is:
- causing symptoms
- 5 to 5.5 cm wide or more
- expanding quite quickly (by more than ½ cm over a six-month period).
Aneurysms between 3 cm and 5 cm should be checked regularly with ultrasound. This monitoring is referred to as ‘surveillance’ or ‘watchful waiting.’
Surgical Procedures
There are two main ways to repair aortic aneurysms:
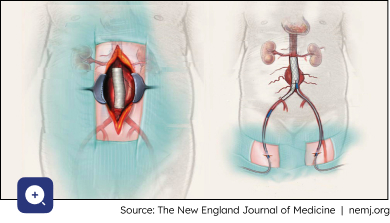
Open surgical repair
- This is the traditional approach, which involves major surgery with a large cut in the abdomen cut to access the affected part of the aorta. The surgery has a lengthy recovery time.
- A special fabric tube (graft) is sewn into place to replace the aneurysm and to recreate a normal-sized blood flow channel.
- Although the operation itself has a higher risk of complications, once you have made a full recovery, the risks of graft-related problems are lower than the risks of the stent placed via the key-hole option.
Endovascular aortic repair (EVAR)
- This is a type of keyhole surgery where the aneurysm is accessed through the leg arteries in both groins. A highly engineered and compressed metal mesh tube, lined with a waterproof fabric (stent-graft), is manoeuvred up to the aneurysm, where it is unfolded to create a reinforced blood flow channel within the aneurysm sac.
- Complications include slipping of the stent-graft from the intended position and leakage of blood back into the aneurysm sac. This is called an endoleak.
- Regular monitoring is required after an EVAR to check for possible post-operative complications.
The overall success rate for these two approaches is similar in experienced hands. The decision about which option is best for you is exceptionally individualised. The vascular surgeons at Cape Town Vascular will carefully assess your personal risks and the detailed anatomy of your aneurysm and guide you on the best course of action.
- Symptoms
- Risks
- Surgical Procedures
What are the symptoms and signs of an aortic aneurysm?
The alarming thing about aortic aneurysms is that most do not cause any symptoms, and many burst with no warning.
When there are symptoms, they are usually:
- Persistent pain in the back (or the sides of the lower back region), belly, or chest. Note: Sudden severe pain in these regions may mean that the aneurysm is about to rupture, especially if you feel faint and sweaty with a fast heartbeat. This is a medical emergency. Do not delay in getting emergency care.
- Noticeable swelling between the ribcage and belly button that pulses in rhythm with your heartbeat.
What increases the risk of an aortic aneurysm?
No single, specific cause has been identified that results in the weakening of the wall of the aorta, but there are several well-known risk factors:
- tobacco smoking – this is the strongest risk factor for aortic aneurysms
- high blood pressure
- age – the risk increases with advancing age, especially in those 65 years and older
- male gender – men are up to six times more likely to have an aneurysm than women
- atherosclerosis (the build-up of fatty plaques within the artery walls) and high cholesterol levels
- family history – if your siblings or parent has or had an aneurysm
- being overweight
- genetic factors or diseases which cause weakness in the walls of arteries.
There are two main ways to repair aortic aneurysms:
Open surgical repair
- This is the traditional approach, which involves major surgery with a large cut in the abdomen cut to access the affected part of the aorta. The surgery has a lengthy recovery time.
- A special fabric tube (graft) is sewn into place to replace the aneurysm and to recreate a normal-sized blood flow channel.
- Although the operation itself has a higher risk of complications, once you have made a full recovery, the risks of graft-related problems are lower than the risks of the stent placed via the key-hole option.
Endovascular aortic repair (EVAR)
- This is a type of keyhole surgery where the aneurysm is accessed through the leg arteries in both groins. A highly engineered and compressed metal mesh tube, lined with a waterproof fabric (stent-graft), is manoeuvred up to the aneurysm, where it is unfolded to create a reinforced blood flow channel within the aneurysm sac.
- Complications include slipping of the stent-graft from the intended position and leakage of blood back into the aneurysm sac. This is called an endoleak.
- Regular monitoring is required after an EVAR to check for possible post-operative complications.
The overall success rate for these two approaches is similar in experienced hands. The decision about which option is best for you is exceptionally individualised. The vascular surgeons at Cape Town Vascular will carefully assess your personal risks and the detailed anatomy of your aneurysm and guide you on the best course of action.