Services | Conditions | Chronic Venous Insufficiency
The Basics
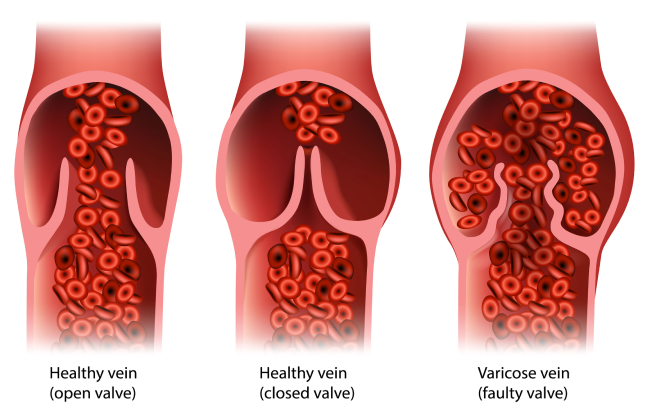
Blood from our legs is returned to the heart via a system of veins. The deep veins run within the leg muscles, and the superficial veins are under the skin. Unlike arteries, which transport blood from the heart to the rest of the body and have a thick muscle layer to regulate flow, the walls of veins are weaker, with only a very thin muscle layer. When you are upright, the challenge is for the venous blood to flow effectively against gravity. Veins have one-way valves to keep the blood moving toward the heart. The leg muscles act like pumps when they contract, e.g. while you walk.
Certain conditions can create a higher-than-normal back pressure in the leg veins. Over time, the compromised venous flow and back pressure leads to chronic venous insufficiency (CVI).
What are the conditions which lead to CVI?
Commonly, the condition is caused by faulty valves in the veins, with resultant ineffective flow of blood from the legs back into the central circulation. Being prone to developing faulty valves increases with age and can run in families or may be the result of damage following a blood clot in the leg, deep vein thrombosis, or a leg injury.
Raised venous pressure may also be due to a blockage in the outflow track of the veins. The most common reason is following an extensive deep vein thrombosis. Other causes include damage from persistent trauma from an overlying artery (May-Thurner syndrome) or external compression from lymphatic glands or other growths in the pelvis.
Any condition that increases the pressure in the abdomen over a long period, making the upward flow of venous blood more difficult, can cause CVI. Examples include excess weight gain and pregnancy.
Risk factors for CVI include:
- History of deep vein thrombosis (most important)
- Varicose veins or a family history of varicose veins
- Obesity
- Pregnancy
- Not getting enough physical activity
- Smoking and tobacco use
- Sitting or standing for lengthy periods
- Sleeping in a chair or recliner
What are the symptoms of CVI?
CVI may manifest as visible varicose veins.
Common symptoms of high venous pressure with poor venous circulation in the legs include:
- Aching, throbbing and tired legs especially after standing for a while and at the end of the day.
- Conditions like oedema or swollen legs develop.
- Skin changes like itching, scaling, and dark or reddish-brown discolouration (haemosiderin staining), especially around the ankle.
- Small cuts that ooze and are slow to heal and which can develop into problem-open ‘venous ulcers.’ These ulcers can take months or even years to close.
What can you do to reduce symptoms for swelling?
- Try to be as active as possible – keep moving to improve circulation.
- Avoid standing or sitting in one position for too long and avoid sitting with your legs crossed.
- When sitting, prop your legs up so your feet are higher than your thighs.
- Wear flat shoes and clothes which are loose around the legs and waist.
- Dropping excess weight will help to reduce the pressure in the leg veins.
For troublesome skin symptoms:
- Wash your legs with unscented aqueous cream or cleanser. Avoid ordinary soaps which can add to the dryness.
- Use the same aqueous cream on your legs just after you have dried them.
What are the treatments for CVI?
Should you and your doctor decide that treatment is required, the options depend on the type of problem veins you have, and your symptoms. The aim of treatment is to relieve symptoms and to tackle the underlying cause of the problem, where possible.
Leg compression is one way to relieve symptoms:
- Graduated elastic compression stockings may form part of your management. They fit tightly over the leg with the most pressure applied around the ankle, with less squeeze exerted the higher up they go. They help the leg muscles push the venous blood back to the heart. While one can buy some brands at the pharmacy, higher-pressure compression stockings require a prescription.
- A common problem is that many people do not find them very comfortable or intolerable, especially in hot weather.
- While leg compression can relieve pressure symptoms like swelling and may prevent progression of skin changes, it does not remove the problem veins.
Medication
In some instances, blood thinners may be appropriate to prevent clots and improve blood flow. Venotonic medications like flavonoids can reduce swelling and ease symptoms.
Surgical Procedures
If the more superficial system of veins is involved, there are several surgical options which can be effective in the management of CVI. These involve reducing venous backflow (reflux) and restoring better circulation. The preferred methods today are minimally invasive, catheter-based techniques, where a catheter (tube) is placed inside the vein to deliver radiofrequency or laser energy to seal the vein. A chemical sclerosant or superglue can also be used to block the vein. These techniques work as well as the open surgical procedures and have the advantage of less pain and bruising and a faster recovery time.
The most common open surgical procedures are:
- Ligation and stripping (Trendelenberg and Strip Procedure): These two procedures are often performed together. For vein ligation, your doctor cuts and ties off the problem veins. Stripping is the surgical removal of larger veins through two small incisions.
- Microincision/ambulatory phlebectomy: This is a minimally invasive procedure. It targets varicose veins near your skin’s surface. Your doctor makes small incisions or needle punctures over your veins. Then, they use a phlebectomy hook to remove the problem veins.
- Vein bypass: This is like heart bypass surgery, just in a different location. Your doctor takes part of a healthy vein from somewhere else in your body and uses it to reroute blood around your damaged vein. Doctors only use this method in severe cases when no other treatment is effective.
Non-Surgical procedures:
- Endovenous thermal ablation: This technique targets large veins. It uses a laser or high-frequency radio waves to create intense heat. This heat closes the diseased vein but leaves it in place so there’s minimal bleeding or bruising.
- Non-thermal endovenous ablation: Uses superglue or a combination of mechanical trauma and sclerosant to close the vein.
- Sclerotherapy: Your doctor injects a foam or liquid solution into your spider vein or varicose vein. This causes the vein to collapse or disappear.
- Vein stenting can be used to open blocked veins.
Vein Disease Stages
CEAP classification: this is a system used to identify the stages of vein disease.

- Symptoms
- Risks
- Surgical Procedures
What are the symptoms of chronic venous insufficiency?
CVI may manifest as visible varicose veins.
Common symptoms of high venous pressure with poor circulation in the legs include:
- Aching, throbbing, swollen and tired legs especially after standing for a while and at the end of the day.
- Skin changes such as itching, scaling and dark or reddish-brown discoloration, especially around the ankle.
- Small cuts which ooze and are slow to heal – and which can develop into problem open “venous ulcers”. These can take months or even years to close up.
What can you do to reduce symptoms for Swelling?
- Try to be as active as possible – keep moving to improve circulation.
- Avoid standing or sitting in one position for too long and avoid sitting with crossed legs.
- When you are sitting, prop your legs up so your feet are higher than your thighs.
- Wear flat shoes and clothes which are loose around the legs and waist.
- Dropping excess weight will help to reduce the pressure in the leg veins.
For troublesome skin symptoms:
- Wash your legs with unscented aqueous cream or cleanser.
- Avoid ordinary soaps which can add to the dryness.
- Use the same aqueous cream on your legs just after you have dried them.
Risk factors for CVI include:
- History of deep vein thrombosis (most important)
- Varicose veins or a family history of varicose veins
- Obesity
- Pregnancy
- Not getting enough physical activity
- Smoking and tobacco use
- Sitting or standing for lengthy periods
- Sleeping in a chair or recliner
If the more superficial system of veins is involved, there are several surgical options which can be effective in the management of CVI. These involve reducing venous backflow (reflux) and restoring better circulation. The preferred methods today are minimally invasive, catheter-based techniques, where a catheter (tube) is placed inside the vein to deliver radiofrequency or laser energy to seal the vein. A chemical sclerosant or superglue can also be used to block the vein. These techniques work as well as the open surgical procedures and have the advantage of less pain and bruising and a faster recovery time.
The most common open surgical procedures are:
- Ligation and stripping (Trendelenberg and Strip Procedure) : These two procedures are often performed together. For vein ligation, your doctor cuts and ties off the problem veins. Stripping is the surgical removal of larger veins through two small incisions.
- Microincision/ambulatory phlebectomy: This is a minimally invasive procedure. It targets varicose veins near your skin’s surface. Your doctor makes small incisions or needle punctures over your veins. Then, they use a phlebectomy hook to remove the problem veins.
- Vein bypass: This is like heart bypass surgery, just in a different location. Your doctor takes part of a healthy vein from somewhere else in your body and uses it to reroute blood around your damaged vein. Doctors only use this method in severe cases when no other treatment is effective.
Non-Surgical procedures:
- Endovenous thermal ablation: This technique targets large veins. It uses a laser or high-frequency radio waves to create intense heat. This heat closes the diseased vein but leaves it in place so there’s minimal bleeding or bruising.
- Non-thermal endovenous ablation: Uses superglue or a combination of mechanical trauma and sclerosant to close the vein.
- Sclerotherapy: Your doctor injects a foam or liquid solution into your spider vein or varicose vein. This causes the vein to collapse or disappear.
- Vein stenting can be used to open blocked veins.