Services | Conditions | Peripheral Arterial Disease (PAD)
The Basics
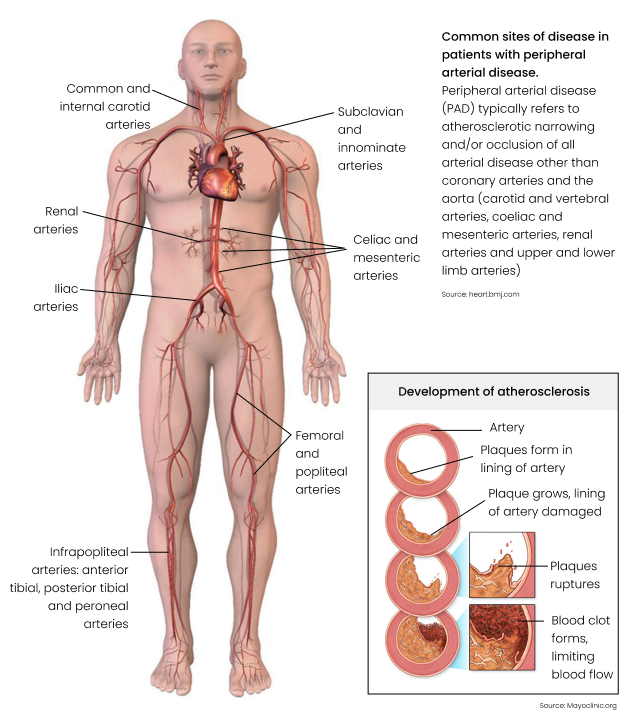
If you have a healthy circulation, oxygen-rich blood flows easily through the arteries to all parts of your body, including the ‘peripheries’ (limbs i.e. arms and legs). Peripheral arterial disease (PAD) is a condition which typically affects the arteries to the legs. They become hardened and narrowed, and the supply of oxygen is reduced. The build-up of fatty deposits in the artery walls usually causes the blockages. These deposits are often referred to as cholesterol plaques. The medical term is atherosclerosis.
What are the symptoms and signs of PAD?
In the early stages of the condition, symptoms occur when there is an increase in the demand for oxygen by the muscle – this happens when you exercise. You experience leg cramps, tiredness, or ‘heaviness’ typically in the buttock, thigh, or calf. The symptoms disappear after resting for a few minutes. Others may experience sexual problems if the arteries to the pelvic organs are affected.
Over time, as the blockages get worse, the reduced circulation and poor oxygen supply can lead to the following:
- wasting of the leg muscles, with weakness
- loss of hair on the leg, thinning skin with colour changes and brittle toenails
- a small scratch can quickly become an infected ulcer which takes a long time to heal
- troublesome burning pain in the feet and toes, when resting, and especially at night in bed
- toes which are numb and cold
With severe PAD, and complete arterial blockage, the area below the blockage (most often the toes) may die off from oxygen deprivation. This is called gangrene, and when it happens, amputation may be required.
What are common conditions which increase the risk of PAD?
- Smoking
- Diabetes
- High cholesterol
- High blood pressure
- Obesity
If you have PAD, you are at risk for developing a heart attack or stroke – caused by the same mechanism, i.e. clogged arteries from atherosclerosis.
How is PAD diagnosed?
Besides your doctor doing a thorough examination, there are several tests which may be done to assist the diagnosis and to locate the site of the blockage:
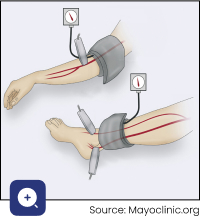
- The ankle-brachial index (ABI) measures the difference in blood pressure in your legs compared to your arms. During this test, blood pressure cuffs are placed on your arms and legs just above the ankle. Blood pressure readings are taken when you are resting and immediately after exercise. The ABI is decreased in a person who has PAD.
- A vascular ultrasound is a non-invasive test used to examine the circulation using a small hand-held device placed on your skin over the area to be examined. An image of the vessel is created and displayed on a monitor. Doppler ultrasound allows one to see the blood flow in the artery.
- An angiogram produces a more precise image of your arteries – a contrast dye injected into the circulation shows up clearly on a CT or MRI scan. This detail may be required if surgery is being contemplated.
What are the treatments for PAD?
PAD is a sign that all your arteries are unhealthy, and although there is no cure, the two central aims of therapy are to:
- Improve your quality of life so that you can be mobile and have fewer symptoms.
- Reduce your risk of serious artery disease complications like heart attack, stroke, and amputation.
There are lifestyle changes that you can make to reduce symptoms and slow the progression of PAD:
- Stop smoking.
- Manage other health conditions which add to your risk, like diabetes, high blood pressure, being overweight, and having high cholesterol.
- Regular exercise is especially important to promote a better circulation – most people with PAD should walk daily.
- Pay attention to good skin and foot care, which will help to prevent infections and ulcers.
Your doctor at Cape Town Vascular will guide you on all these aspects, including how best to begin a walking program.
Medicines
There are several different classes of medicines which are used to manage the underlying causes of PAD, to reduce your risk of even more serious complications of artery disease. Everyone with PAD should, at minimum, be on aspirin to prevent clots, and cholesterol medication, unless there is a particularly good reason otherwise. There are also medications which can help to manage your pain.
Surgical Procedures
In more advanced cases, where lifestyle changes and medications alone are not enough, a ‘revascularisation’ procedure may be recommended to improve the blood flow.
There are two main types of revascularisation operations:
- Angioplasty and/or stenting – during this keyhole procedure, a catheter is used to deliver a balloon or a meshed metal cylinder (stent) to the exact spot where there is narrowing. The balloon is expanded to stretch the narrowing or blockage, or the stent is deployed to open the artery.
- Artery bypass grafting – this involves a major operation where a section of healthy vein or a synthetic vessel is used to bypass the blockage caused by the diseased artery.
Angioplasty is a simpler procedure with faster healing but may not always be advisable or possible. At Cape Town Vascular, our surgeons will carefully explain the benefits and risks of each option. Our surgeons will then recommend the approach best suited for your situation.
- Symptoms
- Risks
- Surgical Procedures
What are the symptoms and signs of PAD?
In the early stages of the condition, symptoms occur when there is an increase in the demand for oxygen by the muscle – this happens when you exercise. You experience leg cramps, tiredness, or ‘heaviness’ typically in the buttock, thigh, or calf. The symptoms disappear after resting for a few minutes. Others may experience sexual problems if the arteries to the pelvic organs are affected.
Over time, as the blockages get worse, the reduced circulation and poor oxygen supply can lead to the following:
- wasting of the leg muscles, with weakness
- loss of hair on the leg, thinning skin with colour changes and brittle toenails
- a small scratch can quickly become an infected ulcer which takes a long time to heal
- troublesome burning pain in the feet and toes, when resting, and especially at night in bed
- toes which are numb and cold
With severe PAD, and complete arterial blockage, the area below the blockage (most often the toes) may die off from oxygen deprivation. This is called gangrene, and when it happens, amputation may be required.
What are common conditions which increase the risk of PAD?
- Smoking
- Diabetes
- High cholesterol
- High blood pressure
- Obesity
If you have PAD, you are at risk for developing a heart attack or stroke, which are caused by the same mechanism i.e. clogged arteries from atherosclerosis.
In more advanced cases, where lifestyle changes and medications alone are not enough, a ‘revascularisation’ procedure may be recommended to improve the blood flow.
There are two main types of revascularisation operations:
- Angioplasty and/or stenting – during this keyhole procedure, a catheter is used to deliver a balloon or a meshed metal cylinder (stent) to the exact spot where there is narrowing. The balloon is expanded to stretch the narrowing or blockage, or the stent is deployed to open the artery.
- Artery bypass grafting – this involves a major operation where a section of healthy vein or a synthetic vessel is used to bypass the blockage caused by the diseased artery.
Angioplasty is a simpler procedure with faster healing but may not always be advisable or possible. At Cape Town Vascular, our surgeons will carefully explain the benefits and risks of each option. Our surgeons will then recommend the approach best suited for your situation.