Services | Conditions | Deep Vein Thrombosis
The Basics
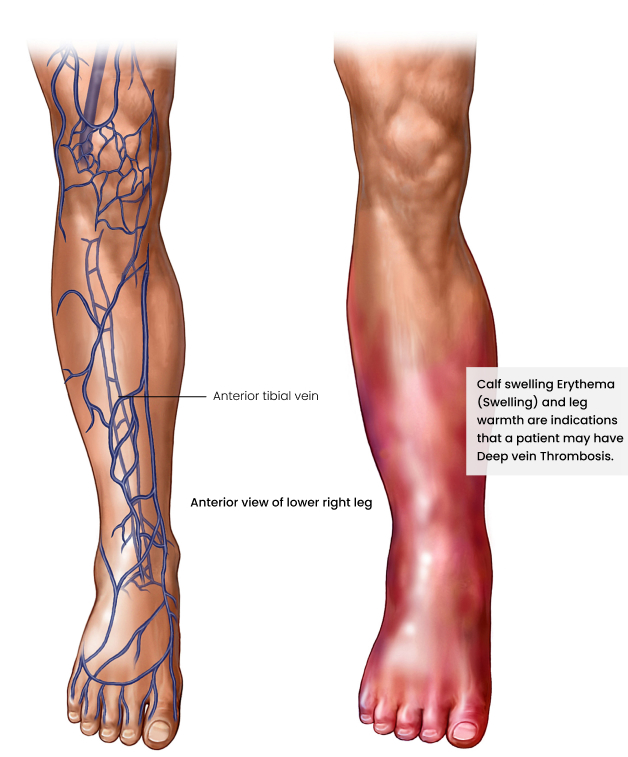
Blood from our legs is returned to the heart via a system of veins. There are deep veins running within the leg muscles, and superficial veins are under the skin. If the deep veins in the legs develop clots, the medical term is deep vein thrombosis (DVT). Smaller clots may go unnoticed and eventually dissolve, but bigger clots block the blood flow. This blockage results in leg swelling and can eventually damage the valves in the veins (which can lead to chronic venous insufficiency). Larger clots are especially dangerous because they can break off and travel via the heart to the lung, where they get lodged. This is called a pulmonary embolism, and it is a life-threatening emergency because it causes a sudden lack of oxygen and sometimes cardiac arrest (when your heart stops beating). Clots can also develop in the deep veins of the arms, but this is uncommon.
What causes DVT?
The ability of blood to clot is essential to prevent excess blood loss when we injure ourselves. However, sometimes blood clots form when they should not.
When problem clotting happens, it is usually a combination of these three underlying factors:
- The normal rate of the blood flow is slowed (stasis).
- The blood vessel walls are damaged and inflamed.
- The usual blood clotting process is abnormally triggered, e.g. inherited clotting disorders.
The blood flow in veins is slower than in arteries, meaning veins are naturally at higher risk of developing clots.
Vein clots commonly form after being immobile in bed because of an operation or injury to the legs or pelvis. Taking blood thinning medication can prevent this from happening.
Another typical scenario is someone with an inherited clotting disorder who has been sitting for hours in a cramped position on a long aeroplane flight without drinking much water (dehydration), where the leg muscles are not working to pump the blood out of the legs against gravity (immobility).
What increases the risk of DVT?
There are several things which are associated with an increased risk of DVT, including:
- a previous DVT
- having close relatives (parents or siblings) who had a DVT
- being pregnant or just having given birth
- being very overweight
- any cause of blockage to the blood flow out of the legs, like a large growth in your groin or lower abdomen or an abnormally narrow vein leading from your leg to your pelvis
- certain kinds of cancer and inflammatory conditions
- hormone medication such as birth control pills and hormone replacement therapy (for menopause symptoms)
- smoking (increases the thickness of the blood)
- having heart failure or certain kidney conditions
- age 60 years or older
What are the symptoms and signs of DVT?
Characteristic symptoms of DVT:
- usually, only one leg is involved
- leg swelling, pain, or cramps
- tightness of the calf area with warm skin, which is reddish or darker than usual, tender with applied pressure
Sometimes, DVT may not cause any symptoms, or only mild symptoms. In some cases, DVT is only diagnosed when it results in a pulmonary embolism. The signs of pulmonary embolism are sudden shortness of breath, chest pain, dizziness or fainting, and feeling anxious and sweaty with a racing pulse.
How is DVT diagnosed?
The two critical diagnostic tests are a duplex doppler ultrasound – where a scanner probe is pressed against your leg to get an image of the veins and the flow within the veins – and a D-dimer blood test. If the D-dimer test is normal, DVT is very unlikely. However, D-dimer levels may be raised in situations besides DVT. Therefore, the combination is useful for a diagnosis. A CT venogram may be required in select cases. This is an imaging test using a specialised CT scan to record detailed pictures of your veins after they are injected with a contrast dye, which shows up on the scans.
What is the treatment for DVT?
Medical treatment, often as an out-patient, is the standard approach. Admission may be required if there is extensive DVT or other specific factors. The goal of medication is to stabilise the existing clot, to prevent clot pieces breaking off, and to thin the blood to prevent new clots from forming. Medication allows the body to break down the existing clot while reducing the risk of pulmonary embolism.
Medicines
Medical treatment is required for three to six months, sometimes even longer, depending on your circumstances. Blood thinners (anti-coagulants) are administered in injectable or tablet form. If you start with an injectable blood thinner, this is usually changed after ten to fourteen days to a tablet form. Tablets may be warfarin, but sometimes another type of blood thinner is prescribed, which requires less intense monitoring. DVT in pregnancy is managed differently, usually with injectable blood thinners until several weeks after birth. Blood thinners have the risk of excess bleeding, and while you are taking them, you should be sure to understand the do’s and don’ts to reduce your risks.
Surgical Procedures
Medical treatment may not be enough by itself. Surgery, typically a keyhole ‘endovenous’ procedure, may be necessary where the big veins of the upper leg and pelvis are involved. ‘Clot-busters’ are injected to break up the clot, which is then suctioned out. Removing the bulk of the clot during the procedure allows for more effective medical therapy, reducing the chances of damage to the vein valves and the longer-term complication of ‘post-thrombotic syndrome’ (chronic venous insufficiency). If it is discovered that you have an abnormally narrow vein, which is creating high back pressures and increasing your DVT risk, a stent can be placed in the narrowing during the same procedure. The stent expands the vein in that area with improved blood flow.
- Symptoms
- Risks
- Surgical Procedures
What are the symptoms and signs of DVT?
Characteristic symptoms of DVT:
- usually, only one leg is involved
- leg swelling, pain, or cramps
- tightness of the calf area with warm skin, which is reddish or darker than usual, tender with applied pressure
Sometimes, DVT may not cause any symptoms, or only mild symptoms. In some cases, DVT is only diagnosed when it results in a pulmonary embolism. The signs of pulmonary embolism are sudden shortness of breath, chest pain, dizziness or fainting, and feeling anxious and sweaty with a racing pulse.
What increases the risk of DVT?
There are several things which are associated with an increased risk of DVT, including:
- a previous DVT
- having close relatives (parents or siblings) who had a DVT
- being pregnant or just having given birth
- being very overweight
- any cause of blockage to the blood flow out of the legs, like a large growth in your groin or lower abdomen or an abnormally narrow vein leading from your leg to your pelvis
- certain kinds of cancer and inflammatory conditions
- hormone medication such as birth control pills and hormone replacement therapy (for menopause symptoms)
- smoking (increases the thickness of the blood)
- having heart failure or certain kidney conditions
- age 60 years or older
Medical treatment may not be enough by itself. Surgery, typically a keyhole ‘endovenous’ procedure, may be necessary where the big veins of the upper leg and pelvis are involved. ‘Clot-busters’ are injected to break up the clot, which is then suctioned out. Removing the bulk of the clot during the procedure allows for more effective medical therapy, reducing the chances of damage to the vein valves and the longer-term complication of ‘post-thrombotic syndrome’ (chronic venous insufficiency). If it is discovered that you have an abnormally narrow vein, which is creating high back pressures and increasing your DVT risk, a stent can be placed in the narrowing during the same procedure. The stent expands the vein in that area with improved blood flow.