Services | Conditions | Carotid Artery Disease and Stroke Prevention
The Basics
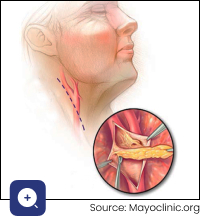
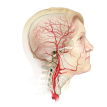
The carotid artery, on each side of your neck, transports oxygen-rich blood from the heart to the brain. The walls of healthy carotid arteries are smooth and elastic. Carotid artery disease is a condition where the arteries become hardened and narrowed. The blockages are caused by a build-up of fatty deposits (cholesterol plaques) in the artery wall. The medical term for these plaques is atherosclerosis. A common site for these blockages is where the common carotid artery branches into the external and internal carotid arteries.
Carotid artery disease can affect the flow of blood to the brain in two main ways:
- A blood clot can form on the surface of the plaque and suddenly block the already-narrowed artery, depriving a part of the brain of oxygen (‘thrombotic’ stroke) or
- blood clot or debris from the heart or plaque in the carotid artery can break off and travel with the upward blood flow to block smaller arteries deep inside the brain (‘embolic’ stroke).
The resultant stroke symptoms can be temporary if the blockage resolves rapidly and blood flow is restored or permanent if the flow is not restored in time to prevent permanent brain damage from sustained lack of oxygen. The condition where stroke symptoms resolve completely within 24 hours is known as a TIA (transient ischaemic attack) or ‘mini-stroke’.
What are the symptoms and signs of carotid artery disease?
Carotid artery disease often goes unnoticed until there is a significant blockage, which results either in a TIA with no permanent brain damage, or a full-blown stroke with permanent disability, or even death.
Sometimes, turbulent flow through a narrowed carotid artery can be detected during a health check by listening with a stethoscope over the neck. The turbulence causes vibrations that make a soft ‘whooshing’ sound in time with the heartbeat. The medical term for this sound is a ‘carotid bruit’.
Signs and symptoms of lack of oxygen to the brain depend on which part of the brain is involved. The following are common:
- Numbness, weakness, or paralysis in the arm or leg on one side of the body
- If the face is affected, it will seem lopsided with drooping of the eye and mouth
- Confusion
- Difficulty speaking and walking
- Disturbances of vision
- Headache, nausea, and vomiting
What increases the risk of carotid artery disease?
The risks of atherosclerosis are the same no matter where in the body the cholesterol plaques develop. If you have a history of angina, heart attack, peripheral artery disease, or aortic aneurysm, you are also at risk of carotid artery disease and strokes.
The commonest risk factors are:
- Smoking
- Diabetes
- High cholesterol
- High blood pressure
- Obesity
- Increasing age and male gender
How is carotid artery disease diagnosed?
Routine screening when there are no symptoms of carotid artery disease does not result in better overall health outcomes in the general population. However, selective screening in certain high-risk groups may be recommended, such as those diagnosed with atherosclerotic disease elsewhere (such as the legs or heart), those with certain risk factors and those with a carotid bruit.
In someone with symptoms compatible with a TIA or stroke, the easiest way to check for carotid disease is with a carotid duplex doppler ultrasound, where an ultrasound probe is pressed against the neck to create images showing the carotid artery blood flow and any blockages.
Other more advanced techniques like a CT angiogram or MR angiogram may occasionally be needed.
Catheter directed cerebral angiography, where dye is injected directly into the carotid artery, is usually only indicated when carotid stenting is being performed.
The diagnosis of carotid artery disease requires an assessment of the degree to which your carotid arteries are blocked. The higher the degree of narrowing, the higher the risk of stroke:
- Minor grade – narrowing of less than 50% of the diameter of the artery.
- Moderate grade – narrowing of 50–69% of the artery.
- High grade (severe) – narrowing of 70% or more of the artery.
What is the treatment for carotid artery disease?
The focus of treatment is stroke prevention.
Lifestyle changes to reduce your stroke risk include:
- Stop smoking.
- Manage other conditions that add to your risk: diabetes, high blood pressure, being overweight, and having high cholesterol.
- Strive to keep up a regular exercise programme.
- Healthy eating to achieve and maintain a healthy weight and waistline.
Medicines
Together with lifestyle measures, medicines may be prescribed, tailored to your risks, e.g. to manage blood pressure, diabetes, or high cholesterol. Typically, you will also have to take low-dose aspirin, which helps to prevent clots from forming. Statins are especially important in decreasing inflammation in the plaque and the risk of stroke.
Surgical Procedures
Consideration for surgery depends on a careful assessment of your individual circumstances, which will allow the surgeon to assess your future risk for stroke and to what extent surgery may reduce this stroke risk.
Factors considered include whether you have previously had a TIA or stroke, the degree of blockage in the carotid artery, your age, and what other medical conditions you have.
Carotid endarterectomy is the preferred surgical option for someone with symptomatic carotid artery disease. During this procedure, the carotid artery is exposed by making a cut in the neck and then exposing and controlling the artery above and below the problem area. The surgeon opens the artery, carefully removes the plaque, and then closes the artery with a patch to keep it wide open.
The surgery carries a risk of complications, such as a stroke (3–6%) and damage to the cranial nerves, which supply surrounding structures like the tongue and the voice box.
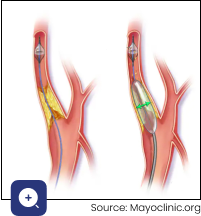
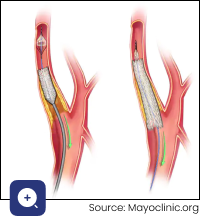
Carotid artery stenting involves accessing the carotid artery, usually from the groin. A guide wire is threaded up to the carotid artery and beyond the blockage, followed by a catheter, which is used to expand a tiny, meshed metal cylinder (stent) at the exact spot where there is narrowing. The stent is expanded to press firmly against the walls of the artery to open it up. This ‘keyhole’ surgery has a higher risk of stroke compared to open surgery, and so is typically only recommended if carotid endarterectomy is not an option and you have a particularly high risk for damaging surrounding structures during an open operation, e.g. post-radiation therapy to the neck.
At Cape Town Vascular, our surgeons keep up to date with the latest scientific guidelines for stroke risk management. The decision to operate depends on the risk versus the benefit and is determined by several factors, including whether there have been symptoms or not, the degree of narrowing, the presence of other medical problems and fitness for surgery, and the patient’s wishes.
We use the most advanced equipment and techniques to ensure the best possible outcomes.
Symptoms | Causes
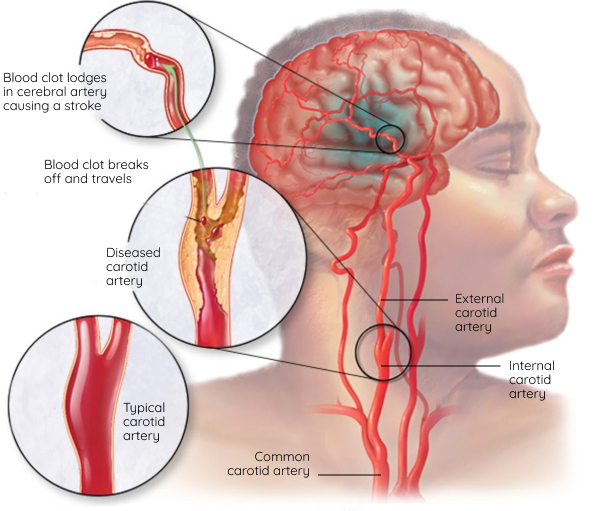
Ischemic stroke
An ischemic stroke occurs when a blood clot, known as a thrombus, blocks or plugs an artery leading to the brain. A blood clot often forms in arteries damaged by a buildup of plaques, known as atherosclerosis. It can occur in the carotid artery of the neck as well as other arteries.
Source: Mayoclinic.org
Diagnosis | Treatment
- Symptoms
- Risks
- Surgical Procedures
What are the symptoms and signs of carotid artery disease?
Carotid artery disease often goes unnoticed until there is a significant blockage, which results either in a TIA with no permanent brain damage, or a full-blown stroke with permanent disability, or even death.
What increases the risk of carotid artery disease?
The risks of atherosclerosis are the same no matter where in the body the cholesterol plaques develop, and if you have a history of angina, heart attack, peripheral artery disease, or aortic aneurism, you are at risk of carotid artery disease and strokes too.
The commonest risk factors are:
- Smoking
- Diabetes
- High cholesterol
- High blood pressure
- Obesity
- Increasing age and male gender
Consideration for surgery depends on a careful assessment of your individual circumstances, which will allow the surgeon to assess your future risk for stroke and to what extent surgery may reduce this stroke risk.
Factors considered include whether you have previously had a TIA or stroke, the degree of blockage in the carotid artery, your age, and what other medical conditions you have.
Carotid endarterectomy is the preferred surgical option for someone with symptomatic carotid artery disease. During this procedure, the carotid artery is exposed by making a cut in the neck and then exposing and controlling the artery above and below the problem area. The surgeon opens the artery, carefully removes the plaque, and then closes the artery with a patch to keep it wide open.
The surgery carries a risk of complications, such as a stroke (3–6%) and damage to the cranial nerves, which supply surrounding structures like the tongue and the voice box.
Carotid artery stenting involves accessing the carotid artery, usually from the groin. A guide wire is threaded up to the carotid artery and beyond the blockage, followed by a catheter, which is used to expand a tiny, meshed metal cylinder (stent) at the exact spot where there is narrowing. The stent is expanded to press firmly against the walls of the artery to open it up. This ‘keyhole’ surgery has a higher risk of stroke compared to open surgery, and so is typically only recommended if carotid endarterectomy is not an option and you have a particularly high risk for damaging surrounding structures during an open operation, e.g. post-radiation therapy to the neck.
At Cape Town Vascular, our surgeons keep up to date with the latest scientific guidelines for stroke risk management. The decision to operate depends on the risk versus the benefit and is determined by several factors, including whether there have been symptoms or not, the degree of narrowing, the presence of other medical problems and fitness for surgery, and the patient’s wishes.
We use the most advanced equipment and techniques to ensure the best possible outcomes.