The Basics
Foot problems affects many people with diabetes. Diabetes-related complications account for 70% of all foot and leg amputations worldwide.
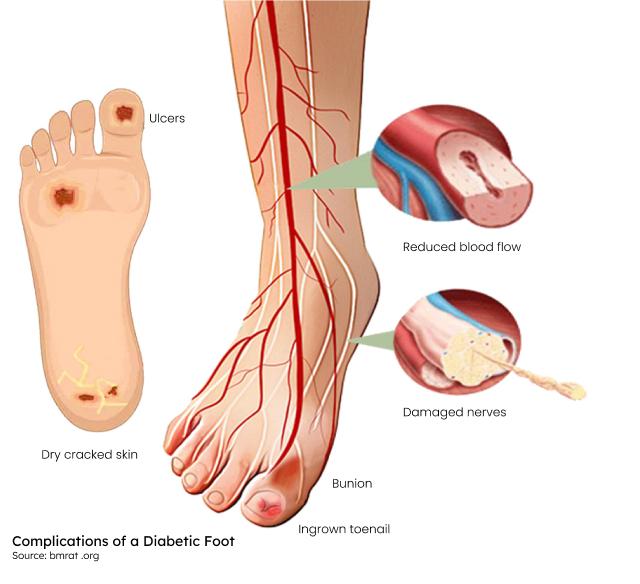
These complications arise due to a combination of three main factors:
- Blockages to the arteries
- Nerve damage
- Infection
Poorly controlled diabetes, with consistently elevated blood sugar (glucose) levels, is very destructive to the tissues of the body, especially the arteries, which over time leads to malfunction in various systems.
Within the walls of the arteries, there is accelerated damage, which results in hardening and the formation of blockages by cholesterol plaques, with reduced blood flow. In the legs, this is called peripheral artery disease. In the most severe scenario, there is complete blockage of the blood flow with death (gangrene) of the affected tissue.
Up to 40% of patients with long-standing diabetic patients also develop nerve damage. The peripheral nerves to the feet and legs are most involved. This nerve damage (called peripheral neuropathy) has several consequences.
These consequences may include:
- Sensory nerve damage leads to loss of the feeling of touch and temperature. One is unaware of small injuries like cuts, burns and blisters, which are usually painful.
- Damage to motor nerves, which supply the foot muscles, causes muscle wasting with resultant deformities like claw toes.
- When the nerves controlling blood flow and sweat glands (called autonomic nerves) are affected, the feet become warm and dry, with cracked skin prone to infection.
High glucose levels impair the immune system. When an impaired immune system combines with poor circulation and inattention to sores on the feet, the result is compromised tissue. This tissue becomes an ideal medium for infection, which can develop rapidly and be challenging to manage.
The combination of poor circulation, nerve damage, and infection can result in a chronic diabetic foot ulcer (DFU), which may result in an amputation.
Risks
Risk factors include:
- poorly managed diabetes
- a foot ulcer in the past
- nerve damage
- poor circulation
- foot deformities, sometimes caused by diabetic neuropathy
What decreases the risk of diabetic foot disease?
The short answer is, good blood sugar control, going for regular foot checks, and educating yourself about how best to take care of your feet – and being consistent in applying what you learn, including guidance on appropriate skin care and wearing suitable shoes. If you have peripheral artery disease, a referral to a vascular surgeon is advised for an assessment to determine if you are a candidate for a procedure to improve circulation.
What are the symptoms and signs of the diabetic foot?
- Although peripheral neuropathy leads to a loss of protective sensation in the feet, one of the most troublesome symptoms is burning foot pain, usually worse at night.
- The feet have poor circulation, and the skin is discoloured, dry, and itchy and susceptible to repeated fungal and bacterial infections.
- Open sores are common and take ages to heal.
- Repeated injuries and changes to the structures within the foot following nerve damage lead to progressive joint destruction and a misshapen foot that increases the risk of further injury (Charcot foot).
How is it diagnosed?
The best way to be sure of a timely diagnosis, which can prevent complications of a diabetic foot, is to go for regular screening checks even if your feet feel fine. Your doctor will examine for deformities or infection and carefully check the nerve and blood supply of your feet. Early changes can be diagnosed with careful sensitivity checks of your feet even before you may be aware there is a problem. As always, prevention is the best medicine. If you have diabetes, you should have a thorough foot exam at least once a year as part of your comprehensive check-up, and if you have already had diabetes-related foot problems, you will have to have check-ups more often. Your doctor will advise you how often you should see them.
What are the treatments for the diabetic foot?
Once you have developed complications related to the diabetic foot, you need to be extra vigilant about new symptoms and sores and do not delay seeking advice from your doctor. You will rely on a team of healthcare professionals to assist you in preserving the function of your feet and legs, e.g. your family doctor, podiatrist, endocrinologist or physician, and a vascular surgeon. You should consult a vascular surgeon if you have a history of infected ulcers or peripheral artery disease. Lifestyle changes can reduce the symptoms and slow the progression of peripheral artery disease.
Offloading
Patients with a non-healing wound of the foot need to take complete pressure off that area. This is known as ‘offloading.’ This is achieved with a combination of a pressure-relieving moon boot or a specialized plaster cast, shoe inserts (orthotics), specialized shoes and other walking aids. This aspect of treatment is essential to heal an ulcer. Diabetic foot ulcers will not heal if pressure is not relieved, even if the circulation is normal and there is no infection.
Surgical Procedures
The surgical treatment of the infection consists of pus drainage and removal of all necrotic and infected tissue.
This type of surgical treatment is called debridement. Debridement is a procedure to clean dead or infected skin and tissue from a foot ulcer. It allows your doctor to assess the extent of the soft-tissue damage and encourage healing. Debridement is a procedure used to clean out dead or infected skin and tissue from a foot ulcer. It allows your doctor to assess the extent of the soft tissue damage and encourage healing. To perform this procedure, a doctor uses a sharp tool, such as a scalpel, to remove tissue from within and around the wound.
Orthopaedic foot surgery may be necessary to correct deformities to prevent pressure ulcers from forming.
Vascular surgery
In patients with poor circulation, it may be necessary to do a procedure to bring blood back to the foot for the wound to heal.
At Cape Town Vascular, we take a special interest in managing the problems which affect the legs and feet of our patients who have diabetes, with the goal of preserving normal function and mobility.
- Symptoms
- Risks
- Surgical Procedures
What are the symptoms and signs of the diabetic foot?
- Although peripheral neuropathy leads to a loss of protective sensation in the feet, one of the most troublesome symptoms is burning foot pain, usually worse at night.
- The feet have poor circulation, and the skin is discoloured, dry, and itchy and susceptible to repeated fungal and bacterial infections.
- Open sores are common and take ages to heal.
- Repeated injuries and changes to the structures within the foot following nerve damage lead to progressive joint destruction and a misshapen foot that increases the risk of further injury (Charcot foot).
Risk factors include:
- poorly managed diabetes
- a foot ulcer in the past
- nerve damage
- poor circulation
- foot deformities, sometimes caused by diabetic neuropathy
What decreases the risk of diabetic foot disease?
The short answer is, good blood sugar control, going for regular foot checks, and educating yourself about how best to take care of your feet – and being consistent in applying what you learn, including guidance on appropriate skin care and wearing suitable shoes. If you have peripheral artery disease, a referral to a vascular surgeon is advised for an assessment to determine if you are a candidate for a procedure to improve circulation.
The surgical treatment of the infection consists of pus drainage and removal of all necrotic and infected tissue.
This type of surgical treatment is called debridement. Debridement is a procedure to clean dead or infected skin and tissue from a foot ulcer. It allows your doctor to assess the extent of the soft-tissue damage and encourage healing. Debridement is a procedure used to clean out dead or infected skin and tissue from a foot ulcer. It allows your doctor to assess the extent of the soft tissue damage and encourage healing. To perform this procedure, a doctor uses a sharp tool, such as a scalpel, to remove tissue from within and around the wound.
Orthopaedic foot surgery may be necessary to correct deformities to prevent pressure ulcers from forming.
Vascular surgery
In patients with poor circulation, it may be necessary to do a procedure to bring blood back to the foot for the wound to heal.
At Cape Town Vascular, we take a special interest in managing the problems which affect the legs and feet of our patients who have diabetes, with the goal of preserving normal function and mobility.