The Basics
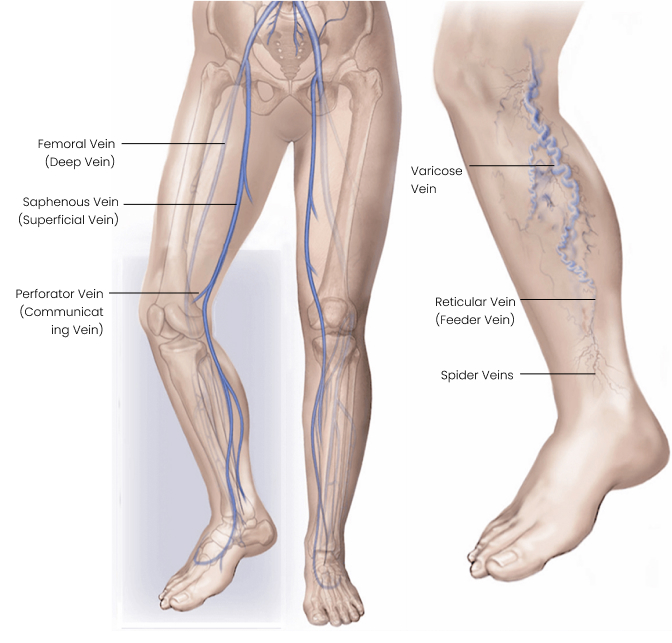
Certain conditions can create increased back pressure in the leg veins. Over time, this constant abnormal pressure can make the veins close to the skin surface become swollen and winding. Abnormal visible veins are part of the superficial system of veins. Doctors classify these veins in terms of their size.
- ‘Spider veins’ or telangiectasia are clusters of small hair-like veins (less than 1 mm in diameter) visible just under the skin. They are very common and occur in 80% of the population. These are harmless but may be unsightly.
- Reticular veins are bluish and a bit bigger, 1–3 mm in diameter. These veins are very common and harmless, but they may be considered unsightly and a source of unhappiness for the affected person.
- Varicose veins are bigger than 3 mm in diameter. They can present like folded blueish cords, which may be bulging.
What conditions lead to varicose veins?
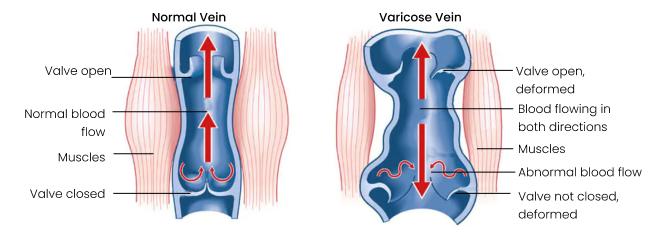
Commonly, varicose veins are caused by faulty valves which allow backflow. Being prone to developing faulty valves increases with age and can run in families or may be the result of a blood clot in the leg or a leg injury, which damages the veins and their valves. Excess weight gain and pregnancy both create extra pressure in the abdomen, making the upward flow of venous blood more difficult. Over time, this can lead to varicose veins. During pregnancy, the walls of the veins also become weaker, which increases the chances of varicose veins.
Risks
Factors that increase your risk of developing spider veins and varicose veins include:
- Age – Ageing causes wear and tear on the valves in the veins that help control blood flow.
- Sex – Women are more likely to develop the condition.
- Pregnancy.
- Family history – Your family members have spider veins or varicose veins.
- Weight – Being overweight or obese.
- Standing.
- Sedentary lifestyle.
- Hormonal changes – The hormonal fluctuations experienced during pregnancy and around the time of menopause.
Symptoms
What are the symptoms of spider veins?
Spider veins usually do not cause symptoms.
What are the symptoms and signs of varicose veins?
Most patients with varicose veins have very few or no symptoms. The symptoms are usually worse at the end of the day because of the increased pressure, and feel much better when the legs are elevated or if elastic compression stockings are worn. Patients can experience:
- non-specific aching, throbbing, tired, itchy, restless legs, especially after standing for a while and at the end of the day.
- swelling of the ankles and feet.
- spontaneous bleeding from the varicose veins.
- superficial thrombophlebitis (inflammation and clotting of the varicose veins).
- worsening of eczema (inflamed, itchy, red rash).
- darkening of the skin especially around the ankle (haemosiderin staining) and inflammation and hardening of the skin (lipodermatosclerosis).
- small cuts that ooze and are slow to heal and which can develop into problem-open ‘venous ulcers’. These ulcers can take months or even years to close.
Treatment options
General measures:
- Elevate the legs when sitting or lying down, as this decreases pressure in the veins and can make the legs feel more comfortable and reduce swelling.
- Exercise. Although the veins may look bigger after exercise because they dilate to increase the flow of blood back toward the heart, exercise does not make the veins worse. Exercise is good for decreasing pressure in the veins, as every time the calf muscles contract, they act as a pump and move blood back to the heart and reduce pressure.
- Avoid long periods of standing still in one place.
- Maintain a normal bodyweight.
- Look after your skin. Moisturize regularly. Dry skin will be more itchy and more likely to crack, allowing germs to enter and set up infection, and to develop ulcers.
- Activities like taking hot baths, or crossing legs when sitting do not play any role in the formation of varicose veins.
Leg compression:
- Graduated elastic compression stockings may form part of your management. They fit firmly over the leg with the most pressure applied around the ankle, with less squeeze exerted the higher up they go. They help the leg muscles push the venous blood back to the heart.
- The stockings need to be a certain strength. Varicose veins usually require a class 2 stocking (30mmHg at the ankle).
- The stockings need to be properly fitted. If they are too loose, they will not work. If they are too tight, they will be too uncomfortable. If too long and folded over, they can act as a tourniquet and potentially cause harm. Do not use old stockings or someone else’s stockings before checking with your doctor or nursing sister that they are appropriate.
- Stockings, if tolerated, are good at making the legs feel more comfortable, controlling swelling and preventing skin changes from getting worse, and preventing ulcers from returning.
- Problems with stockings include:
- Many people find them very uncomfortable or intolerable, especially in hot weather.
- They are difficult to put on and take off, which is a major problem in elderly, immobile and arthritic patients.
- They do not take away the underlying veins.
- Patients with blockages to the arteries that bring oxygen to the leg may not be able to tolerate stockings, and they can even cause harm.
- Skin allergy to the stockings.
Surgical Procedures
Endovenous
The preferred methods today use endovenous or minimally invasive, catheter-based procedures. The main vein with non-functioning valves is punctured with a needle using ultrasound guidance. A fine catheter is passed up the vein to within 2 cm of where it joins the deep system. This vein is then sealed so that there is no flow or pressure being transmitted to the large branches (varicose veins). There are different types of catheters, which either use heat (radiofrequency or laser), superglue, or a combination of trauma to the inside of the vein and a chemical (pharmaco-mechanical).
This procedure takes care of the underlying problem. It is usually combined with phlebectomies or sclerotherapy to take care of the large, unsightly varicose veins.
The advantage of endovenous techniques over traditional open surgery is less pain and bruising and quicker recovery and return to normal activities.
Open surgery
Traditional open surgery involves disconnecting the non-functioning superficial vein from the deep system and stripping the vein from the leg (e.g. Trendelenberg and Strip procedure). It is still used in patients who are not suitable for the endovenous technique.
Sclerotherapy
Another treatment is injection sclerotherapy. During treatment, a chemical sclerosing solution is injected into the affected veins. The injection irritates the inside of the vein, and over time, the vein will collapse and fade from view. A programme of repeat injections is often needed to get to the desired outcome.
Spider veins can be treated with micro-sclerotherapy, or laser sclerotherapy, or a combination of both, depending on the size of the vessels.
- Symptoms
- Risks
- Surgical Procedures
What are the symptoms of spider veins?
Spider veins usually do not cause symptoms.
What are the symptoms and signs of varicose veins?
Most patients with varicose veins have very few or no symptoms. The symptoms are usually worse at the end of the day because of the increased pressure, and feel much better when the legs are elevated or if elastic compression stockings are worn. Patients can experience:
- non-specific aching, throbbing, tired, itchy, restless legs, especially after standing for a while and at the end of the day.
- swelling of the ankles and feet.
- spontaneous bleeding from the varicose veins.
- superficial thrombophlebitis (inflammation and clotting of the varicose veins).
- worsening of eczema (inflamed, itchy, red rash).
- darkening of the skin especially around the ankle (haemosiderin staining) and inflammation and hardening of the skin (lipodermatosclerosis).
- small cuts that ooze and are slow to heal and which can develop into problem-open ‘venous ulcers’. These ulcers can take months or even years to close.
Factors that increase your risk of developing spider veins and varicose veins include:
- Age – Ageing causes wear and tear on the valves in the veins that help control blood flow.
- Sex – Women are more likely to develop the condition.
- Pregnancy.
- Family history – Your family members have spider veins or varicose veins.
- Weight – Being overweight or obese.
- Standing.
- Sedentary lifestyle.
- Hormonal changes – The hormonal fluctuations experienced during pregnancy and around the time of menopause.
Endovenous
The preferred methods today use endovenous or minimally invasive, catheter-based procedures. The main vein with non-functioning valves is punctured with a needle using ultrasound guidance. A fine catheter is passed up the vein to within 2 cm of where it joins the deep system. This vein is then sealed so that there is no flow or pressure being transmitted to the large branches (varicose veins). There are different types of catheters, which either use heat (radiofrequency or laser), superglue, or a combination of trauma to the inside of the vein and a chemical (pharmaco-mechanical).
This procedure takes care of the underlying problem. It is usually combined with phlebectomies or sclerotherapy to take care of the large, unsightly varicose veins.
The advantage of endovenous techniques over traditional open surgery is less pain and bruising and quicker recovery and return to normal activities.
Open surgery
Traditional open surgery involves disconnecting the non-functioning superficial vein from the deep system and stripping the vein from the leg (e.g. Trendelenberg and Strip procedure). It is still used in patients who are not suitable for the endovenous technique.
Sclerotherapy
Another treatment is injection sclerotherapy. During treatment, a chemical sclerosing solution is injected into the affected veins. The injection irritates the inside of the vein, and over time, the vein will collapse and fade from view. A programme of repeat injections is often needed to get to the desired outcome.
Spider veins can be treated with micro-sclerotherapy, or laser sclerotherapy, or a combination of both, depending on the size of the vessels.